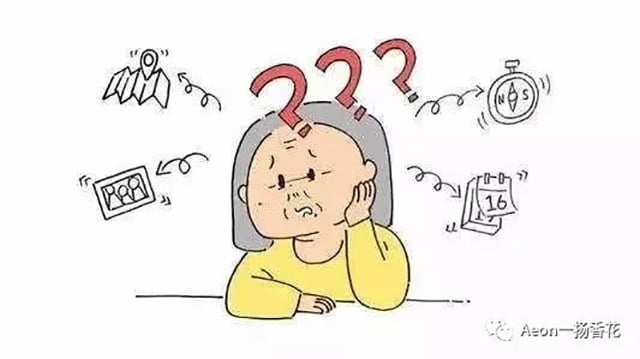
Alzheimer’s Disease (AD), denoted as Alzheimer’s Disease or AD, is a progressive neurodegenerative disorder commonly affecting older adults. It significantly impairs cognitive function, memory, behavior, and sleep, yet the exact cause remains unknown. The disease typically progresses over years or even decades, causing immense suffering for patients and their families, and imposing a massive economic burden on society. Currently, the global cost of caring for AD patients stands at a trillion dollars, projected to reach two trillion by 2030, with an average survival post-diagnosis often less than six years. This poses a severe threat to the health of elderly individuals. As China, a populous nation, is forecasted to have more AD cases by 2040 – equal to the combined total of all advanced countries – the implications of this issue are substantial.

As the aging population intensifies, the prevalence of AD is anticipated to surge. Consequently, studying and addressing AD treatment and care holds significant importance in enhancing patients’ quality of life and reducing familial burdens. Researchers posit that AD’s pathogenesis encompasses synaptic loss, damage to acetylcholine-producing neurons, aggregation of β-amyloid protein (Aβ), the neurovascular hypothesis, and the vestibular hypothesis.
However, there is currently no available drug that can effectively decelerate or prevent neuronal damage in AD. Most conventional treatments cannot reverse the disease’s structural changes, and they may present heightened adverse effects for elderly patients. Despite extensive previous research, pharmaceutical efforts to develop new drugs for AD treatment have largely fallen short, highlighting the ongoing challenges in finding effective solutions for this debilitating condition.
In recent years, non-pharmacological interventions have garnered significant attention for their potential in mitigating and ameliorating AD symptoms and pathology. Among these, aromatherapy, a popular non-drug approach both domestically and internationally, has demonstrated multiple benefits, including improved sleep quality, reduced negative emotions, and enhanced cognitive function. This study, through a review of relevant literature, provides an overview of aromatherapy, delves into its underlying mechanisms, and explores its application in AD patients. Its aim is to contribute theoretical foundations for non-pharmacological AD management and serve as a reference for the broader use of aromatherapy in treating AD patients.
The Mechanisms of Aromatherapy in Treating AD
Essential oils used in aromatherapy are generally recognized for their neuroprotective properties, helping to reduce the toxic effects of amyloid beta (Aβ) on the brain and serving as an effective tool for mitigating neurological impairments. In contrast to oral medications, aromatherapy offers a route of administration that bypasses the gastrointestinal system, thus providing a potentially safer option. While a consensus on the exact mechanisms is still evolving, the impact of olfactory stimulation on an individual’s emotions, physiology, and behavior is widely accepted as a key aspect in understanding how aromatherapy operates.

Research indicates that AD patients exhibit varying degrees of olfactory dysfunction, with numerous interconnected brain regions in the olfactory cortex and hippocampus, such as the amygdala, perirhinal cortex, olfactory bulb, and entorhinal cortex, playing a direct role in the process of olfactory memory. These areas are activated upon receiving olfactory stimuli, affecting the flow of information required for higher-level tasks like olfactory recognition and memory. Functional magnetic resonance imaging studies have observed that odor stimulation activates the amygdala and hippocampus, with the latter linked to memory functions. The amygdala in the limbic system, crucial for emotion regulation and memory, also contributes to these processes.
Findings suggest that odors and music can evoke more vivid emotional experiences and accelerated memory recall in AD patients, signifying that odors can act as memory triggers. From a psychological perspective, it is believed that individuals’ reactions to smells are linked to emotional associations, giving them a characteristic emotional valence that elicits cognitive, behavioral, and physiological responses congruent with their previous emotional experiences. This aligns with the neuroanatomy of the limbic system, where olfactory processing is intricately connected to neural structures involved in emotion and memory processing.

From a pharmacological standpoint, the interaction between various scents and internal factors influences the endocrine and nervous systems. Essential oils and their components possess diverse pharmacological activities, such as analgesic, anxiolytic, and anticonvulsant effects. They are employed to treat patients with anxiety, insomnia, seizures, pain, and cognitive impairments through inhalation or oral administration. The underlying mechanism likely lies in the ability of essential oils and their compounds to modulate the γ-aminobutyric acid (GABA) system and sodium ion channels, thereby exhibiting protective, anxiety-reducing, and anti-seizure properties.
Application of Aromatherapy in AD (Alzheimer's Disease)
Cognitive function
Cognitive decline is a prominent symptom in AD patients, and studies have shown that aromatherapy has significant therapeutic effects on cognitive improvement. Aromatherapy can enhance cognitive function by targeting different cognitive domains. Japanese researcher Jimbo et al. conducted a study on 28 AD patients, where they applied rosemary mixed with lemon essential oil in the morning and lavender blended with orange oil at night, using a fan to disperse the fragrances. Results indicated an improvement in cognitive function scores for the participants.
In China, current research on aromatherapy’s impact on cognition mainly focuses on basic studies. Chinese scholars have discovered that active components in jasmine flowers can increase excitability of neurotransmitters in the hippocampus, stimulating damaged nerves and promoting repair of neurons in the hippocampus. Consequently, aromatherapy can facilitate olfactory function and reinforce memory recovery. Research involving AD animal models has revealed that lavender essential oil can eliminate excessive reactive oxygen species, maintaining the brain’s redox balance, and improving serum biochemical markers and protein expression related to oxidative stress, ultimately contributing to enhanced memory function.

Behavioral and psychiatric symptoms
AD patients often exhibit behavioral and psychological symptoms of dementia (BPSD), for which there are currently no特效药物. Antipsychotic medications are commonly used to manage mental and behavioral symptoms in dementia patients, but BPSD can significantly degrade their quality of life. Long-term use of antipsychotics can lead to resistance and may cause side effects such as sleep disturbances, extrapyramidal symptoms, cerebrovascular events, and increased mortality risk.
Aromatherapy is frequently utilized in AD patients, particularly for improving mental and behavioral symptoms. Oils like chamomile, lavender, ylang-ylang, and rosemary have been shown to help reduce agitation in AD patients. Lin’s study recruited 70 AD patients, reporting that three weeks of lavender oil inhalation effectively alleviated agitation. This suggests that aromatherapy is suitable for patients who are vulnerable to adverse effects of psychiatric medications, offering fewer side effects and better tolerance compared to conventional treatments. Furthermore, it can ease caregivers’ stress and improve their mood alongside AD patients.
Some researchers combine aromatherapy with methods like massage and music to enhance the therapeutic effects. For instance, Turtun Kaymaz and colleagues found that concurrent aromatherapy inhalation and massage can mitigate agitation in AD patients, thereby reducing caregiver burden. However, it is essential to conduct scientific studies to determine the most effective combinations and optimal intervention durations.

The quality of sleep
There is evidence establishing a connection between AD and sleep disorders. Poor or good sleep quality is considered a critical factor influencing the development and progression of AD. Traditionally, AD is thought to provoke sleep problems, with the severity of insomnia correlating with dementia’s progression. Sleep disturbances caused by AD can directly contribute to the accumulation of amyloid-beta (Aβ) proteins, leading to neurodegeneration. Conversely, sleep disorders themselves may also promote protein deposition associated with neurodegeneration.
Amyloid-beta plaques, a hallmark of AD, exhibit circadian fluctuations in soluble amyloid levels in mice and humans, underscoring the significance of sleep in clearing Aβ. Cross-sectional studies have reported sleep issues in 25% to 35% of AD patients. Johannessen and his team conducted a three-month aromatherapy intervention on 24 AD seniors residing in a nursing home, concluding that aromatherapy not only reduces medication reliance but also improves sleep quality by decreasing nightmares and nocturnal awakenings.
Hwang and others analyzed 13 studies through a systematic review, confirming the positive impact of aromatherapy on patient sleep. Seven of these studies combined aromatherapy with other techniques like massage, providing a model for combining various non-pharmacological interventions. Overall, these findings suggest that aromatherapy can be a valuable addition to the management of sleep disturbances in AD patients.

Palliative care
For severely advanced AD patients approaching the end of their life, aromatherapy aims primarily to enhance their end-of-life quality and bring comfort to both patients and their families. Hu Chunyan’s research found that incorporating essential oils into massages increases patient comfort and positively impacts therapists and caregivers. Göpferth et al. conducted a trial on 10 healthy individuals, 15 conscious terminal patients, and 5 unconscious terminal patients, using vital signs and oxygen saturation measurements as evaluation criteria. Although they did not observe statistically significant results, they concluded that aromatherapy could help alleviate psychological stress in terminal patients and reported no severe adverse effects during the therapy. This encourages healthcare professionals and caregivers to consider using aromatherapy in home care or palliative settings.
Currently, there are very few clinical studies applying aromatherapy in palliative care. Further large-scale randomized controlled trials and qualitative research are needed to confirm its efficacy in this context.
Adverse reactions
A systematic review of aromatherapy for Alzheimer’s Disease (AD) patients found that among the 12 clinical trials analyzed, only 4 specifically reported adverse effects. It was mentioned that while aromatherapy generally carries no dangerous complications, there is a possibility of adverse reactions when certain essential oils are used extensively over time or applied topically. These may include skin irritation or allergic dermatitis. It is crucial to consider the quality and safety of the oils, as well as the patient’s allergy history and tolerance, before selecting an appropriate oil and method of use.

other
Ballard et al. used the Dementia Care Customization (DCM), a quality assessment tool for dementia care, to observe the impact of aromatherapy on the quality of life of AD patients and found that patients in the aromatherapy group spent more time participating in social activities than those in the control group. Yang et al. recruited 59 AD patients and were randomly divided into an intervention group and a control group. The intervention group received a 30-minute aromatherapy massage once a week. After 8 weeks, the overall depressive symptoms of the intervention group were significantly reduced as the intervention time increased.
Summary and outlook
Since the number of AD patients remains high and there is currently a lack of effective drug treatments, it is crucial to explore economical, safe, and effective non-drug intervention methods to improve patients’ quality of life and slow down the progression of the disease. Aromatherapy can improve the cognitive function of AD patients, relieve mental and behavioral symptoms, and improve sleep quality. The method of stimulating olfactory nerves through fragrance exposure is low-invasive and easy to implement, making it suitable not only for AD patients but also for caregivers. This review once again confirms the potential of aromatherapy as a non-drug intervention in the treatment of AD patients, and it is a valuable option worthy of widespread use in medical institutions, communities, and families.
In the future, we hope that more high-quality research will confirm the effectiveness of aromatherapy from the following aspects:
1) Research scope: In the future, it is expected that more research on aromatherapy in AD can be carried out simultaneously in families, communities, and medical institutions in order to achieve the best research results;
2) Research content: Future research can quantitatively analyze the effects of essential oil components selected for aromatherapy and combinations of different proportions on AD patients, with a view to energizing and standardizing the selection of essential oils.
3) Research type: Animal experiments can clarify the effects and mechanisms of essential oils on human studies, which is a necessary condition for determining the pharmacological basis of aromatherapy. In the future, it is expected that more aromatherapy research will combine the biology and clinical application of AD patients to bridge the gap between preclinical evidence and clinical results.